The correct answer is A. This patient's presentation is classic for disseminated gonococcal disease. Disseminate gonococcal disease begins as a migratory arthritis and evolves into a purulent monoarthritis. Fever, elevated WBCs, and genitourinary symptoms are variable. Necrotic papules on the extremities can be a valuable clue to the diagnosis. The patient's history of unprotected sex and dysuria should provide further clues to diagnosis. NAAT (nucleic acid amplification test) is recommended on the first urine in the morning in order to make this diagnosis. Health care providers should culture the rectum, cervix, urethra, and pharynx as well as obtain blood cultures if a drug resistant strain of gonorrhea is suspected. Initial treatment with ceftriaxone is now recommended as first-line treatment. Typically, this is accompanied with a single one gram of azithromycin. Parenteral antibiotics are typically given for 7 days. . It would also be prudent to cover for the possible coexisting Chlamydia infection with the single dose of azithromycin.
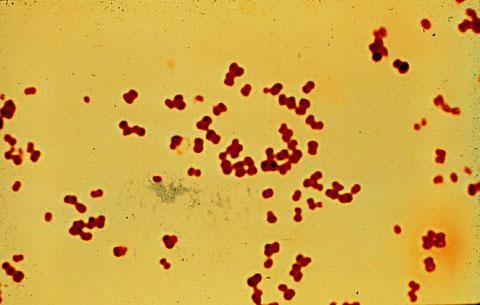
Nafcillin (choice B) is the first-line agent for staphylococcal septic arthritis. Our patient's history strongly suggests gonococcal arthritis and the synovial fluid Gram stain further supports the diagnosis.
Gonococcal penicillin-resistance is becoming increasingly prevalent, so penicillin is not an appropriate initial antibiotic (choice C) . Historically, penicillin was first-line treatment, but this is no longer the case.
Vancomycin (choice D) should be reserved for patients who are at risk for methicillin-resistant Staphylococcus aureus, such as IV drug users, nursing home patients, or in-patients who acquired the infection in the hospital. Vancomycin is not utilized in the treatment of gonococcal disease.
Withholding antibiotics (choice E) is incorrect. Septic arthritis can be very destructive to the involved joint. Patients who have septic joints must be admitted to the hospital and treated aggressively and quickly with antibiotics. Waiting for culture results can be dangerous and could result in permanent joint damage.
PEARL: Gonorrhea can lead to systemic symptoms such as polyarthritis, which indicates disseminated disease. The joints most commonly involved include the wrists, ankles, and small joints of the hands and feet. Signs of disseminated disease can also include conjunctivitis, fever, and skin lesions at the extremities. Treatment includes ceftriaxone (Rocephin) plus a single one-gram dose of azithromycin
Disseminated gonococcal infection (DGI) is the most common cause of acute nontraumatic monoarthritis or oligoarthritis in young adults. Patients who have DGI typically present with one of 2 syndromes:
- A triad of tenosynovitis, vesiculopustular skin lesions, and polyarthralgias without purulent arthritis
- Purulent arthritis without associated skin lesions
Gonococcal arthritis is a common cause of septic arthritis in which the organism cannot be cultured on routine culture media. Cultures of synovial fluid tend to be positive in <50% of cases of gonococcal arthritis. Because of this, a negative synovial culture does not rule out gonococcal arthritis.
Affected adults are sexually active individuals and typically present with fever, chills, skin lesions, polyarthralgias, and tenosynovitis evolving into a persistent monoarthritis or oligoarthritis.
The joint aspirate should be cultured for N. gonorrhoeae when the history is suggestive. NAAT of the first morning voided urine can prove that gonorrhea is present. The yield can be increased if plates of chocolate agar or Thayer-Martin medium are inoculated with synovial fluid at the bedside along with cultures from clinically appropriate sites (e.g., the pharynx, urethra, cervix, rectum, and skin lesions). Blood cultures are often positive in patients who have DGI presenting with tenosynovitis and skin lesions alone, but are frequently negative if a joint effusion is present. The infected fluid is usually purulent with an average leukocyte count (most of which are neutrophils) of 50,000ndash150,000 cells/mm3. The likelihood of septic arthritis increases with rising synovial fluid leukocyte count.
Nucleic acid hybridization tests and nucleic acid amplification tests (NAAT) are now generally recommended as the first-line method of testing. Urine, urethral, cervical, and vaginal specimens can be utilized.